A new research project has been awarded over £6m to develop a toolkit to allow 3D printed medicines to be manufactured effectively bringing innovations like biological personalised pills and ‘living plasters’ closer to commercial production.
The EPSRC funded five-year project is a collaboration being led by researchers from Engineering and Pharmacy at the University of Nottingham, alongside the Universities of Cambridge, Reading and Strathclyde.
The teams will work together develop a toolkit that will allow industry to identify, select and process the correct materials to 3D print into new regenerative medicines and pharmaceuticals.
Professor Ricky Wildman from the University of Nottingham’s School of Engineering is leading the project and explains: “There is currently a lack of agility in UK manufacturing preventing 3D printing being developed in certain areas of industry. Manufacturing needs the capability to quickly, predictably, and reliably ‘dial up’ performance to produce products embedded with advanced functionality.
“Many pharmaceutical firms don’t know how to go from concept to reality with 3D printing. They aren’t sure what materials are 3D-printable, or which order to combine the materials or what function different geometric profiles have. This new project aims to provide all of this information to enable commercial application.”
Using computational modelling and machine learning the team will develop instructions for use by industry to accelerate the development cycle of new drugs, which could reduce timescales from two years to six months.
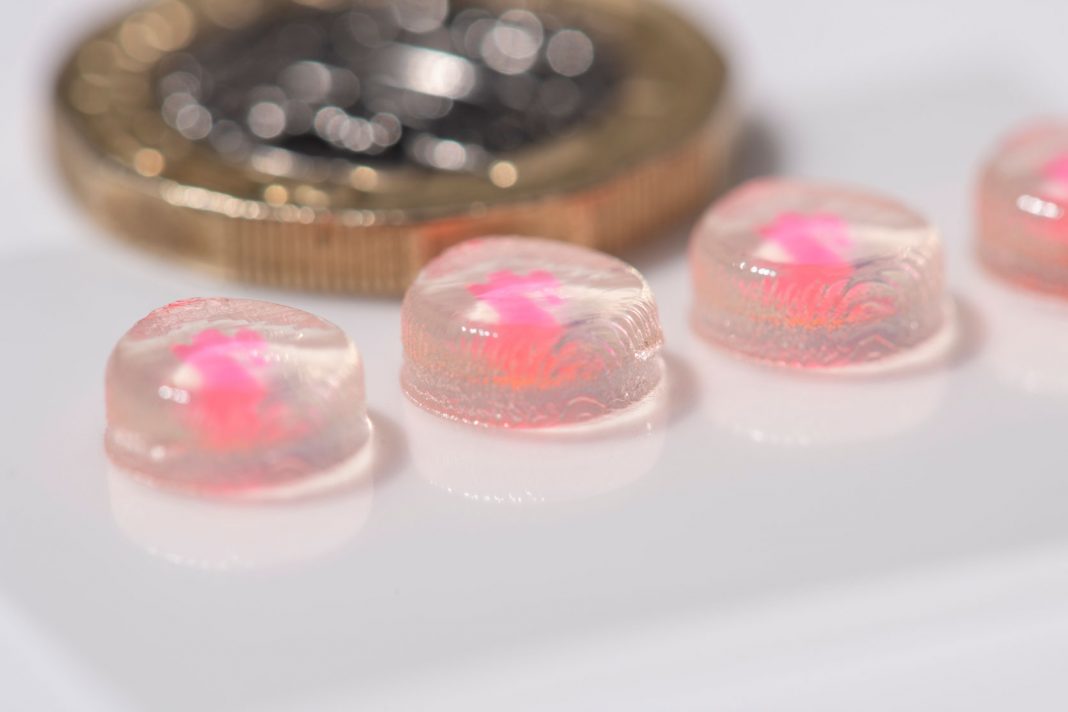
As part of the project three test pharmaceutical products will be developed and tested, all of which rely on the incorporation of proteins or enzymes to promote cell growth and have customisable, complex and multi-material requirements.
The team are testing a biological pill that could potentially replace injected vaccines. The 3D printed personalised pill could be posted to the patient and taken easily, cutting out issues with logistics, delivery and administering of the drug.
An intestinal patch or ‘living plaster’ is also being developed that could calm inflammation potentially helping patients with Crohn’s or bowel disease. The plaster would be laid over the internal area and release active ingredients to help heal and support cell renewal.
Professor Clive Roberts from the University of Nottingham’s School of Pharmacy adds: “Whilst these products are in their infancy we are hoping to be able to develop these innovations to demonstrate the capabilities of the 3D printing tool kit and be able to show how we can combine materials to provide personalised medicines that are safe, effective and low cost.”
“This is very exciting work which, through building cellular models, will improve our understanding of how the gut functions,” said Professor Mohammad llyas, a consultant at NHS Nottingham. “More importantly, if successful, it will lead to a paradigm shift in clinical management and launch the use of autologous tissue-engineered therapeutics for the treatment of bowel disease.”